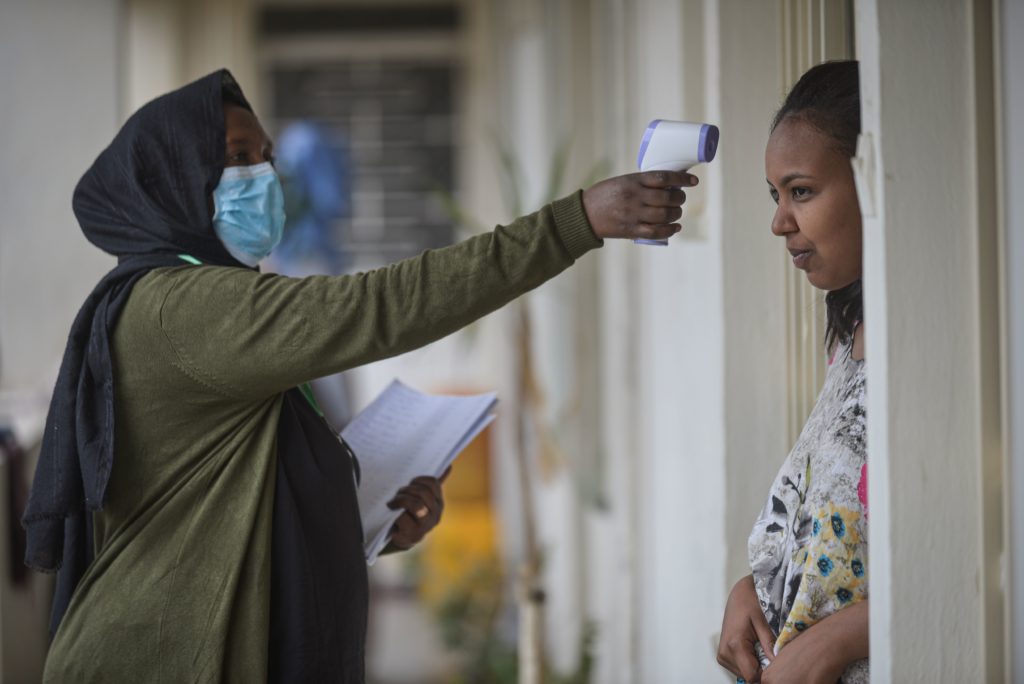
Report: Poor Policies Contributed to Spike in Unintended Pregnancies and Unsafe Abortions at the Height of COVID-19 Pandemic in Five African Countries
NAIROBI, 19 May 2022– A new report reveals that women and girls from households living on lower incomes in five African countries faced multiple barriers in accessing sexual and reproductive health (SRH) services at the onset of COVID-19 pandemic.
The study also sought to examine how healthcare providers, women, girls, and individuals in the LGBTQI+ community in Burkina Faso, Ethiopia, Kenya, Malawi, and Uganda responded to offering and seeking services at the height of the pandemic. People in underserved communities often experienced limited access to contraceptives, maternal health care, abortion care, and HIV/AIDS prevention and management. Based on interviews with 3473 women and girls, and 446 health providers, the study showed that care-seeking was often delayed postponed or forgone altogether.
The report, Impact of COVID-19 Pandemic on Sexual, and Reproductive Health Services in Burkina Faso, Ethiopia, Kenya, Malawi, and Uganda, further reveals that the pandemic resulted in an increase in unintended pregnancies, sexual and gender-based violence, unsafe abortions, and preventable maternal and infant deaths. Additionally, individuals in the LGBTQI+ community and persons with disabilities (PWDs) experienced challenges in accessing reproductive healthcare.
The study attributes the poor reproductive health outcomes to government policies that failed to strike a delicate balance between containing the spread of COVID-19 pandemic and addressing the reproductive health needs of women, girls, and LGBTQI+ individuals. Most health facilities closed and others were converted to isolation and treatment centers. Healthcare providers were often redeployed to COVID-19 units and reproductive health supplies were deprioritized. The study makes several recommendations.
Evelyne Opondo, Senior Regional Director for Africa, Center for Reproductive Rights (CRR) said: “At all times, reproductive health services remain essential. The rights of entire populations to access sexual reproductive health services, including during the pandemic, remain a key responsibility of every government. Governments must accord the highest protection of reproductive rights for women, girls and individuals in the LGBTQI+ community.”
Boniface Ushie (PhD), Research Scientist at African Population and Health Research Center (APHRC), said: “Government policies in response to health emergencies must be continuously reviewed to ensure they effectively respond to evolving trends and developments.”
Victor Rasugu, Executive Director, Network for Adolescent and Youth of Africa (NAYA) said: “With fears that COVID-19 might become endemic, we can no longer afford to ignore essential interventions in other aspects of healthcare. Local and national governments must strengthen community health outreach to enhance adolescents and youth access to reproductive health information and services.”
L. Achieng Akumu, Esq. Africa Regional Director, Planned Parenthood Global (PPG) said:“Governments must supply private health facilities with reproductive health commodities to adequately serve the vulnerable women, girls and sexual minorities.”
Nelly Munyasia, Executive Director Reproductive Health Network Kenya (RHNK) said: “Governments must institutionalize inclusive, client-friendly trainings and sensitization of health providers to ensure effective service delivery in the wake of pandemics.”
Dr. Ernest Nyamato, Global Associate Director, Quality of Care at Ipas said: “Healthcare providers must be supplied with personal protective equipment (PPEs) to cushion them from the pandemic and psychological stress emanating from operating in such crisis contexts.”
Dr. Shiphrah Kuria, Reproductive Maternal, Child and Adolescent Health Expert at Amref Health Africa said: “Governments must adopt holistic responses and recovery strategies that access impacts of pandemics in different socioeconomic sectors.”
Other additional findings include:
- Access to SRH information: 48%of women and girls across the study countries received information from friends; 29% received information from the internet; and less than 10% received information from teachers.
- Access to and uptake of SRH services: 26% of women and girls across the study countries could not access modern contraceptives; Burkina Faso (47%) recorded the least access. Most sought-after services included contraceptives (46%), followed by antenatal care (40 %). Post-abortion care/PAC (3%) was the least sought-after service during the pandemic.
- Access to contraceptives: 58% of women and girls across the study countries received short-acting contraceptive methods, while 35% received long-acting reversible contraceptive methods.
- Barriers to SRH services: Women and girls across the study countries could not access services due to myriad factors: restricted movements (61%), closure of health facilities (13%), excessive costs (18%), long distances (24%).
- Coping with barriers to SRH services: 46% of women and girls delayed seeking services. Another 21% of women and girls visited a different health facility or a health provider, while 19% never visited a health facility. Uganda recorded the highest delays number of women and girls who delayed seeking services (63%).
- Availability of SRH services: Health facilities across the study countries lacked medical abortion supplies. Burkina Faso (26%) was the most affected followed by Kenya (18%), Uganda (12%) and Ethiopia (5%). Kenya (72%) was the most affected with stock out of Mifepristone/misoprostol, followed by Uganda (48%), Burkina Faso (23%) and Ethiopia (20%). Uganda was the most affected with stock out of contraceptive implants, followed by Kenya (19%), Ethiopia (6%), and Burkina Faso (9%).
- Continuity of SRH services during pandemic: Ethiopia (75%) and Burkina Faso (74%) trained the highest number providers, while Ethiopia (84%) and Kenya (77%) supplied the highest number of personal protective equipment/PPEs.
- Unavailability of some services: Providers in Burkina Faso (100%) did not offer post-abortion care/PAC due to stock-out of commodities and absence of trained healthcare staff. Providers in Uganda (83%) did not offer post-abortion care/PAC due to stock-out of commodities only. In Kenya and Ethiopia, services were not offered due to lack of trained providers and absence of patients.
###
MEDIA CONTACT: Kennedy Arthur Wekesa, [email protected]